The purpose of the showcase is to promote and publicize excellence in medical device design by teams of undergraduate and graduate students conducted as part of their course work and provide a unique networking opportunity.
This is a competition and student teams are being evaluated during the event. The top three teams will be announced at the conclusion of the event and receive one of three cash prizes.
Novel Device Design for Large Ovarian Cyst Removal (Grand Prize Winners)
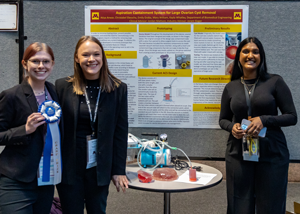
Worldwide 7% of women have an ovarian cyst; this jumps to 18% for postmenopausal women in the USA. A cyst is an accumulation of fluid or substance in a pocket of tissue. Both the ovary and the follicle within the ovary are prone to forming cysts when eggs are released. Some ovarian cysts can resolve on their own, but many require surgical removal. Ovaries are composed of the only tissue in the body that can expand with essentially no limit, allowing cysts to grow beyond the normal ovary size. Ovarian cysts may also be cancerous. 21,000 women in the US annually have ovarian carcinomas, causing 14,600 deaths.2 In order to determine if a cyst is cancerous, surgical removal is required as CT scans and transvaginal ultrasounds provide limited indication. Ovarian cysts are often removed without determining if it is cancerous. If a cancerous cyst leaks its contents during removal, cancer cells could be spread to other parts of the body and necessitate the patient undergoing chemotherapy. Surgeons assume that the cyst contents are dangerous to the patient and use methods to avoid spilling the contents of the cyst during the surgery.
Student Team: Atiya Anwar, Christobel Ekeocha, Emily Graba, Mary William, and Kayla Whatley
University of Minnesota
Portable Fluid Warmer Design for Use in Austere Environments (2nd Place Winners)

The Air Force Special Operations Command (AFSOC) Medical Modernization Office and Air Force Research Lab (AFRL) 711th Human Performance Wing (HPW) tasked the Mechanical Engineering, Biology, and Chemistry Departments at the United States Air Force Academy (USAFA) with designing a multi-functional fluid warming device for reliable use in operational settings. When special operators need to infuse blood or other fluids into a patient in the field, they typically carry very cold (1-6°C) blood products. Current technologies for portable fluid warmers often do not provide an adequate flow rate and/or do not increase the temperature of the fluid to threshold values when used in field settings. This can cause the patient to experience either hypovolemic or hypothermic shock, respectively. This degree of blood loss in a trauma patient can quickly escalate to a life-threatening situation
Student Team: William Mockel (C1C), Brigid Barkmeier (C2C), Elizabeth Cassidy (C2C), Emma Dershem (C2C), Matthew Lee (C2C), Kelly Yoon (C2C), and Joshua Coya (C3C)
U.S. Air Force Academy
Advisors: Lt Col Ilea Heft, U.S. Air Force Academy, Department of Biology
Col Wilfred Delacruz, U.S. Air Force Academy, Department of Biology
Capt Damon Kirkpatrick, U.S. Air Force Academy, Department of Mechanical Engineering
Novel Surgical Device to Repair a Dural Defect via the Transmastoid Approach (3rd Place Winners)
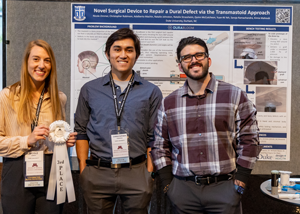
DuraBloom is the first surgical tool capable of both easily elevating the dura 360o around the defect and deploying a graft between the bone and dura to seal the CSF leak via the transmastoid approach. Surgeons simply position DuraBloom within the defect and push a slider on the handle of the device to separate the dura from the bone and insert a graft. After the graft is in place, the surgeon can then move the slider back, leaving the graft behind to seal the defect and repair the CSF leak.
Student Team: Nicole Zimmer, Christopher Robinson, Adalberto Machin, Natalie Strassheim, Quinn McCutcheon, Yuan-Ni (Sydney) Yeh, Natalie Johnston, Saroja Ramachandra, and Kimia Mahboub
Biomedical Engineering, Duke University
Accessory Curette Instrument for Orthopedic Oncology Application
Tumors within the bone often require extraction utilizing specialized tools such as a curette. A bone curette is used to scrape away tumor tissue in the hopes that healthy bone will grow back and fill the space occupied by the removed mass. In some patients, orthopedic surgeons may combine curettage with a bone graft or implant within the cavity to fill the void. However, when observing curette use, the instrument is a rigid fixed-angle device that in some cases requires inefficient handling and awkward positioning. This complication can lead to insufficient tumor tissue removal, and specific indications for curettage such as giant cell tumor(s) of bone (GCT) are associated with high rates of recurrence when utilized without adjuvant treatment. When these tumors grow back, one hypothesis to their recurrence is insufficient tissue removal. Therefore, the problem addressed with this device is incorporating the dexterity of the surgeon’s fingers with the curette to increase the amount of tumor removed.
Student Team: Zachary Mendoza, Brandon and Look Fong
Texas A&M University, Department of Engineering Medicine
Device for Sequestered Thrombolysis using Targeted Thrombolytic Drug Delivery
The issues with the current approaches to clot removal (mechanical thrombectomy and pharmaceutical thrombolysis) make it challenging to identify which option is the right fit for the patient. A better solution should include a simplified procedure with only one device to save time and prevent damage, as well as a clearly laid out design and set up, according to Dr. Jagadeesan of the University of Minnesota, and Curtis Goreham-Voss, an engineer at Switchback Medical.
Student Team: Elliot James, Heather Breidenbach, Mia Tran, Rachana Sangem, Roudra Bhattacharya, and Sadhika Prabhu
Department of Biomedical Engineering, University of Minnesota
SPLiTO2: Mechanical Device Delivering Oxygen to Multiple Patients Simultaneously
SPLiTO2 serves as a medical device to address the global oxygen shortage and widespread CRD by: 1- splitting oxygen into multiple channels, allowing treatment for multiple patients simultaneously, 2- supplying independent, high-range and accurate oxygen flows, and 3- featuring a low-cost design with parts locally manufacturable in SSA. The SPLiTO2 is expected to increase oxygen therapy access in low-resource areas, globally. Likewise, SPLiTO2 will fill the specific market need for reliable oxygen delivery to patients in low-resource regions of SSA. SPLiTO2’s core function is to input high-flow oxygen from a single source, such as a cylinder, and redistribute flow to many patients simultaneously.
Student Team: Hannah Bockius, Meghan Bolt, Mickayla Harris, Cliff Lowan, Erika Siegel, and Hayley Sussman
University of Delaware, Department of Biomedical Engineering
Advisors: Professor Julie Karand, Professor Sudesh Sivarasu, Sarah McEwan
CervX Device For Treatment of Cervical Insufficiency
An estimated 1% of expectant mothers experience preterm labor due to cervical insufficiency, accounting for 20% of mid-second trimester spontaneous pregnancy loss.1 Cervical insufficiency is characterized by weakening of cervical muscles, causing dilation and subsequent preterm birth. Preterm birth can have adverse effects on the child and expectant mother, including bleeding, infection, higher risk of long-term health problems, and postpartum depression. Current treatments include cervical cerclage, a stitch around the cervix, combined with a cervical pessary, a cone shaped device inserted into the vaginal canal to support. While being the standard of care, it is estimated that 1 out of 50 patients have complications due to a cervical cerclage, including bleeding and fetal loss. Our proposed medical device is an non-invasive alternative to a cervical cerclage to minimize these factors. The CervX device consists of a zip tie mechanism coated in silicone to provide an adjustable, easy to install clamping mechanism for the cervix to prevent cervical insufficiency complications. The side touching the cervix is ridged to provide extra friction so the device will not slip off, and the zip tie can tighten to accommodate natural variation in cervix size.
Student Team: Athanacia Papoutsis, Sumeet Thosar, Neha Panigrahy, and Rahul Ramanathan
University of Illinois Urbana-Champaign
Acknowledgments: Jen Smith, Gies, Dr. Aaron Traeger M.D. (Gies College of Business MBA Student)
BAMBI: A Biointelligent Apnea Monitor for Bradycardia Prone Infants
Our project has three primary objectives: 1) reduce the subjectivity in apneic event identification, 2) automate the first and second lines of infant stimulation, and 3) facilitate better data reporting to physicians. As a secondary objective, we also wanted our system to integrate with commonly seen NICU setups.
Student Team: Pallavi Jonnalagadda, Grace Qian, Jessica Ling, and Ria Dawar
University of Pennsylvania
A Method to Improve Measurement of Intraoperative Femoral Version Correction
We have come up with an electromechanical approach that addresses both segment fixation and intraoperative rotational measurement. Segment fixation is achieved using an external fixator assembly comprised of a series of semicircular rings that rotate relative to each other to accomplish the required rotation.
Student Team: Olivia Coder, Dominic Rivas, and Andrew Behrens
Department of Biomedical Engineering, University of Iowa Roy J. Carve
Late-Stage Posterior Glottic Stenosis Intervention
The goal of the design is to restore vocal fold mobility to allow sufficient glottal area for comfortable respiration. To improve mobility, a small prosthetic joint that can be inserted between the cricoid and arytenoid cartilages has been designed. This joint is intended to return rotational movement to the arytenoid, allowing for the abduction of the vocal folds by mimicking the articulating surfaces of the joint. Using a cast developed from a mold of cadaveric arytenoid and cricoid cartilage, a thermoplastic prototype was developed. The curved side of each implant articulate on each other simulating the natural saddle-like joint. The goal of the design is to restore vocal fold mobility to allow sufficient glottal area for comfortable respiration. To improve mobility, a small prosthetic joint that can be inserted between the cricoid and arytenoid cartilages has been designed. This joint is intended to return rotational movement to the arytenoid, allowing for the abduction of the vocal folds by mimicking the articulating surfaces of the joint. Using a cast developed from a mold of cadaveric arytenoid and cricoid cartilage, a thermoplastic prototype was developed. The curved side of each implant articulate on each other simulating the natural saddle-like joint motion. The flat side of the two implants are attached to the existing cartilage. Using 3D scanning software, a digital model was created of the cartilages. This model will be used to develop and test further prototypes.
Student Team: Joseph, Marissa McFadden, Sofia Peraza, and Noah Sinclair
Roy J. Carver Department of Biomedical Engineering, University of Iowa
Collaborators: Dr. Matthew Hoffman, UIHC Department of Otolaryngology, Dr. Edward Sander, UI College of Engineering, Roy J. Carver Department of Biomedical Engineering
Brainwaves: Medical Device for the Simplification of Pediatric Polysomnograms
Our proposed solution is a design that consists of an integrated housing encapsulating a cleaning gel, abrasive tape, conductive paste, and allows easy insertion of a 10mm disc electrode. This “all-in-one” solution reduces the many steps involved in the current system setup and speeds up the overall process while providing more consistent results than the current methods used. The device comes pre-assembled with all components listed in the Bill of Materials in Figure 1, excluding the electrode. This allows sleep labs to continue using their current/preferred electrode and requires minimal preparation from the technician prior to patient arrival for a study. To begin, the technician will load their electrode into the top slot of the device as shown in Figure 2. They will then remove the bottom-most tab to release 0.02mL of cleaning gel through an abrasive cleaning tape. The cleaning tape can then be slid back and forth through the device to clean the precise area where the electrode will be placed, avoiding cleaning too large of an area which can also negatively impact signal collection. After cleaning, the other two tabs are removed exposing the conductive paste. The top cap is then pushed down, sliding the electrode into contact with the paste and then the scalp. The device reduces the setup time by combining the separate steps of the current practice and easily integrates with all other devices in use in the sleep lab setting. This integrated housing will be used in combination with a simple cap that stretches to fit over the patient’s head and features holes in the 10-20 electrode placement locations required for the polysomnogram. These holes allow for easy access to the EEG electrode placement locations and use of the integrated housing in these locations.
Student Team: Kathryn Garn, Kaira Lujan, Jhalak Mehta, and Vanessa Salinas
Bioengineering, Rice University
SIMBA: A Simulated Environment for Neonatal Cardiac Tamponade
The design that has been set forth has been tested in numerous ways to ensure that it meets all functional requirements and functions as required. The device aims to provide a simulation for neonatologists to practice pericardiocentesis to treat cardiac tamponade. Therefore, all testing determined if the device could simulate cardiac tamponade properly.
Student Team: Sam Baule, Shadi Shariff, Nicole Stubbe, and Julia Wizeman
Department of Biomedical Engineering, University of Iowa
Compact and Low-Cost Device to Locate the Trachea in Thick-Neck Patients for Emergency Cricothyrotomy
Our approach to solving the problem is by building a handheld, inexpensive ultrasound device that utilizes signal processing to detect the soft tissue barrier created by the walls of the trachea, similar to how a stud finder locates a nail. This method eliminates the need for the physician to interpret the ultrasound reading which can same time and energy during this stressful procedure.
Student Team: Thijs Larson, Claire Westman, Mitch Kowalke, MC Arvidson, John Carlson, and Jared Snidarich
Department of Biomedical Engineering, University of Minnesota
Otoseal: Design and Analysis of Pneumatic Otoscope Speculum Tip Sealants
Acute otitis media (AOM) is a middle ear infection that occurs behind the tympanic membrane. AOM is misdiagnosed in about 50% of pediatric cases. AOM can be diagnosed using a traditional otoscope, but can be hard to accurately diagnose from visual assessment alone. The pneumatic otoscope is the gold standard tool used to diagnose AOM because it can assess both the inflammation and mobility of the TM. However, because of differences in ear canal shape compared to the circular shape of a traditional speculum tip, improper speculum sizing, or fidgeting patients, it is difficult to achieve a proper seal using the pneumatic otoscope. This results in poor visualization of the tympanic membrane and difficulty in diagnosis of pressure-specific conditions such as otitis media or tympanic membrane perforation.
Student Team: Alexandra Farhangui, Kajol Shah, and Sindhura Sridhar
School of Engineering Medicine, Texas A&M University
Yoro: A Fully 3D Printable Prosthetic Arm
This device has an enormous range of motion. Starting from the fingers, they are divided into three phalanges each with a proper anatomical ratio and an equivalent range of curling motion. Each finger is the same length to simplify manufacturing and assembly but are staggered at the base to improve aesthetic. The base also allows for sideways motion, allowing the fingers to splay and grab larger objects. The thumb is similarly designed but with a larger range of motion at the base, allowing it to swivel 360°. Digits are manually positioned by the user’s existing hand and rely on friction to hold their posture. Altogether, the four fingers can support roughly 8lbs of weight before the friction is overcome. Each joint is connected by a metal binding barrel; the adjustable tightening of the barrels creates the frictional force in each joint. The next iteration will replace these with printed joints.
Student Team: Finn Witt
McKelvey School of Engineering, Washington University in St Louis
PanCam - Panoramic Camera Design for the Detection of Colorectal Cancer
Colorectal cancer (CRC) is the fourth most common type of cancer in the U.S.A. and is the second leading cause of cancer death, with an estimated 52,500 deaths in 2022.1 According to Dr. Satish Singh, a practicing gastroenterologist at Boston VA Medical Center with over 20 years of experience, anal cancer prevalence is increasing albeit difficulty in screening may under-represent these values. Early indications of these cancers are large (>1cm) or multiple polyps in the patient’s colon or rectum.2 These polyps often manifest without noticeable symptoms in the patient, therefore it is important for individuals to get screened for CRC regularly.
Student Team: Naimah Gill, Krish Kapadia, Sarah Sheng, and Ksenija Tasich
Boston University
Automated Leveling of Powered Wheelchairs to Decrease Traveling Time
Conditions such as Spinal Muscle Atrophy and Cerebral Palsy, among others, can affect one’s ability to move from one place to another on their own. The disease demographic targeted contains approximately 764,000 cerebral palsy patients, 291,000 paralysis patients, and 25,000 spinal muscular atrophy patients1,2,3. In these cases, a powered wheelchair may be used. When a user that has difficulty using their hands operates a powered wheelchair, it is of the utmost importance that their hands remain on the control stick of the wheelchair. If their hand shifts away from the control, they may not have the muscle strength to reposition their hand, effectively losing control of the wheelchair.
Student Team: Justin Bridges, Ethan Custis, Sommer Dorrough, Ethan Dunkin, and Grant Kohls
University of Alabama at Birmingham
A Novel 3D Printable Bioabsorbable Stent to Improve Gastrointestinal Anastomoses
The inSTENT is the first bioresorbable intestinal stent and compressive band combination for safely and effectively creating surgical connections within the gastrointestinal (GI) tract. Traditional methods of reconnecting intestine segments following resections within the GI tract are associated with alarming leakage and mortality rates. The patent-pending inSTENT device can be used to reconnect intestinal segments without staples, sutures, and the risks and consequences of intestinal leakage. The inSTENT is completely bioresorbable, meaning that after healing takes place, both the stent and the band will be degraded and absorbed by the body, eliminating the need for an additional surgical procedure to remove the device.
Student Team: Clara Black, Brandon Lou, Gillian Pereiram, and Ziming Ye
University of Washington
Competition Judges
Will Durfee, University of Minnesota - Competition Chair
Jessica Falcone, NIH
Andrew Hansen, VA Medical Center
Danny Sachs, University of Minnesota
Dawn Bardot, Abiomed
Roger Sheldon, Bakken Medical Devices Center
Mithun Suresh, CentraCare
Pat Dillon, MNSBIR, Inc
Doug Frans, University of Minnesota
Carl Nelson, Univeristy of Nebraska
David Black, Schwegman, Lundberg & Woessner
Mary MacCarthy, University of Minnesota
Alena Talkachova, University of Minnesota
Steven Saliterman, University of Minnesota
Vaughn Schmid, University of Minnesota
Ibrahim Yekinni, Bakken Medical Devices Center
Daniel Mooradian, University of Minnesota
Carla Pavonne, University of Minnesota
Dan Broberg, Bakken Medical Devices Center
Matt Johnson, University of Minnesota
Marge Hartfel, Bakken Medical Devices Center
Gregory Peterson, University of Minnesota