The purpose of the showcase is to promote and publicize excellence in medical device design by teams of undergraduate and graduate students conducted as part of their course work and provide a unique networking opportunity.
This is a competition and student teams are being evaluated during the event. The top three teams will be announced at the conclusion of the event and receive one of three cash prizes.
Teams added as they are confirmed.
Adaptable Below-the-Knee Pediatric Prosthesis (Grand Prize Winners)
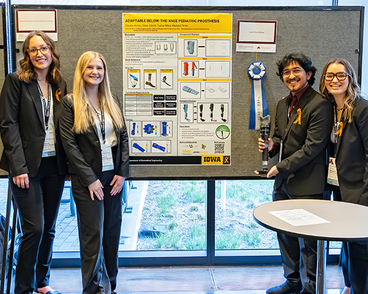
Pediatric patients with below-the-knee prostheses often undergo recurrent adjustments to these devices due to rapid growth. In the United States, congenital limb differences occur in one out of every 1,900 newborns; almost 150,000 children across the country. Children’s prolonged growth spurts, extending across several years, demand multiple modifications or replacements. Ill-fitting prostheses can lead to various complications such as skin irritation, gait irregularities, postural changes, and increased stress on the contralateral side of the body. Furthermore, the financial burden of these frequent appointments, adjustments, and replacements are not always alleviated by insurance coverage.
While prior art focuses on modifying different segments of a prosthesis, there are few options out there that are all encompassing for the adjustment of, both, the height and width. Therefore, our team developed GroLimb: a design to simplify the adaptive fit process of a pediatric below-the-knee prosthesis in response to growth.
University of Iowa Student Design Team:
Clàudia Archer, Claire Catlett, Tushar Mitra, and Maddy Timm
DRIPPY: A Gravity Bag Feeding Rate Modulator (2nd Place Winners)
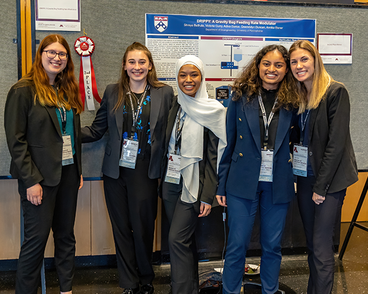
Feeding tubes offer nutrition to over 3 million people globally who are unable to consume food orally or are suffering from malnutrition. Among devices providing non-oral nutrition, there is a need for a regulated feeding rate; variable feeding rates, which may be caused by changes in stomach pressure or user movement, can cause patient discomfort and vomiting. Feeding pumps can circumvent these risks by mechanically pushing fluid at a fixed rate. However, pumps are expensive ($500+ USD) and often inaccessible to those without health insurance. Consequently, many patients must utilize gravity bag feeding. Beyond the limitations surrounding variable drip rate, gravity bag feeding requires the time-intensive process of manual drip rate adjustment every 10-15 minutes from a caregiver through approximately five 20-60 minute feeds per day. In both lower and higher-resourced countries, accessibility of accurate, simple, and consistent feeds remains unaddressed by gravity bags alone. To decrease caregiver stress and improve user safety, Drippy has been designed to detect fluid drip rate and adjust tube compression to ensure rate consistency despite changes in stomach pressure.
University of Pennsylvania Student Design Team:
Shreya Bathula, Victoria Curry, Adiva Daniar, Gwendolyn Duncan, Annika Eisner
Ultrasound Transducer Positioning Aid for Fetal Heart Rate Monitoring (3rd Place Winners)
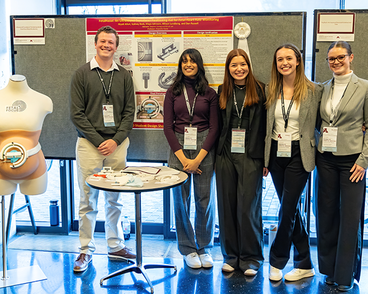
Fetal heart rate monitoring is a critical technique used in the OBGYN practice to provide information about a fetus's well-being during antepartum and intrapartum hospital visits. Currently, there exists an ongoing challenge of losing fetal heart rate signals when the fetus moves leading to critical gaps in data acquisition and prolonged prenatal visits. As a result of these challenges, it has become necessary for fetal heart rate monitoring transducers to be readjusted frequently to reestablish an adequate fetal heart rate signal. While the current transducer attachment mechanism (an elastic band) is simple and inexpensive, it can be difficult and time-consuming to adjust and does not offer proper stability for the transducer. Our device, a wearable positioning aid, aims to solve these issues by allowing healthcare providers to more efficiently and accurately adjust the fetal heart rate monitoring transducer during hospital visits. With this device, the consistency and reliability of fetal heart rate monitoring will be enhanced, thus improving care given to the patient and the fetus.
University of Minnesota Student Design Team:
Niyati Alluri, Sydney Beck, Maya Johnson, Allison Lundborg, and Dan Russell
Advisors: Stephen Contag, M.D. and Shruti Iyer
See-Rynge: A Visually Accessible Liquid Measurement Device

Liquid measurement, a routine in daily life, is effortlessly carried out by a significant portion of the world’s population in activities such as meal preparation and medication administration. However, for the global population of visually impaired individuals, this common practice can be challenging. This challenge is further exacerbated by the absence of visually accessible liquid measuring devices, which forces this community to roughly estimate important measurements or seek assistance, undermining their autonomy and, potentially, their wellbeing. Thus, this project aims to address this widespread issue and offer a solution that is specifically catered for individuals with visual impairments. Our device, See-Rynge, is a liquid measurement tool that features tactile buttons, audio feedback, and a companion app to empower individuals with visual impairments to independently and confidently handle liquid measurements in their daily lives.
University of Pennsylvania Student Design Team: Chiadika Eleh, Joey Wei, Liam Pharr, Isaac Kim, and Venkatesh Shenoy
Development of a Next Generation Intraosseous Needle Medical Device

In emergency situations, the need for immediate vascular access is paramount to survival. In pediatric populations, it is typically very difficult to gain vascular access with an IV line. In those critical scenarios, an intraosseous (IO) needle is drilled into the tibia of the patient to access the marrow cavity (intraosseous space) of bones. IO needles are commonly used, in fact 24% of critical pediatric procedures in the US involve IO access. However, there are two major problems that current IO medical devices do not address: infiltration of fluids into surrounding tissue and needle displacement during patient transport. The infiltration of fluids can cause tissue necrosis and delay life saving medication and as patients are frequently moved around in emergency situations, preventing displacement is integral. We have prototyped a novel needle design that solves both problems and will mitigate risks in pediatric ERs.
University of Minnesota Student Design Team:
Dilshan Rajan, Anuk Dias, and Shaliny Jadhav
TinyTrach: An Improved Neonatal Endotracheal Tube
Endotracheal intubation (ETI) is an extremely common procedure performed when a patient experiences respiratory or cardiopulmonary distress: over 1 million pediatric intubations are performed annually in the U.S. alone. Currently, endotracheal tubes (ETTs) are positioned above a patient’s carina via a physician’s visual estimation and secured with medical tape. Patients can be intubated for weeks at a time and require up to daily X-ray checks to confirm ETT placement. However, pediatric patients have smaller, more sensitive respiratory anatomy, and are easily affected by failed first-pass intubations or prolonged radiation exposure. Misplaced or dislodged ETTs can also lead to scarring, infections, and other complications. Thus, there exists a need to develop a sensor-enabled ETT capable of relaying positioning information and anchoring securely on the patient to reduce ETI complications and expensive, frequent X-ray position checks. Such a device will ensure seamless, painless intubation and reduce pediatric mortality.
Rice University Student Design Team:
Sambhu Balakrishnan, Mina Ghayour, Leighton Less, Shreya Majeti, Abi Parthasarathy, Jack Pearce, and Rian Philip
Scarstretch: A Burn Scar Massaging Device for Pediatric Patients in Costa Rica

Scarring from burns is common, especially in children, and can result in hypertrophic scarring. Scar massaging, a series of motions performed on children by caregivers, is prescribed in low and middle-income countries like Costa Rica. Unfortunately, this process presents a time commitment and burden on caregivers, reducing treatment efficacy. To relieve this burden, we have created ScarStretch, a low-cost, automated wearable scar massaging device. This device consists of three main components: massage head and motor subsystem, attachment mechanism, and controller designed to be easily usable for children and their caregivers. To use, patients or caregivers simply apply the device to the arm and operate with the handheld controller. Preliminary results show promising similarity to hand massage performance and excellent usability.
Rice University Student Design Team:
Shivani Gollapudi, Katie Hart, Pranav Mandyam, Nate Miller, Madison Roy, JJ Tellez, and Zoe Wang
ADONA - Assisted Detection of Neonatal Asphyxia

Hypoxic-ischemic encephalopathy (HIE), a lack of blood flow and oxygen to the newborn brain, is responsible for 23% of neonatal deaths worldwide. The current standard for HIE detection is the grading of electroencephalogram (EEG) data by a specialized neurologist. However, this time and labor-intensive process leaves many infants with delayed or no treatment altogether. Our solution, ADONA, is a non-invasive, streamlined diagnostic aid for the universal screening of HIE. The device features an adjustable, nine-electrode EEG cap with an integrated machine learning algorithm to automatically detect neonatal episodes of HIE.
University of Pennsylvania Student Design Team:
Jude Barakat, Allison Elliott, Daniel Ghaderi, Aditi Ghalsasi, and Taehwan Kim
Quantification of maternal blood loss during Cesarean section

Primary postpartum hemorrhage (PPH) is the leading cause of maternal deaths worldwide. PPH is defined as blood loss of over 1000mL during C-section. Surgeons in low-middle income countries (LMICs) use visual estimation to determine how much blood has been lost, however this technique often leads to underestimation of the true amount lost. When blood is mixed with amniotic fluid, the method becomes even more inaccurate, since the human eye is unable to distinguish pure blood from 50% blood. If detection of PPH is too late, appropriate treatment cannot be given, leading to adverse health outcomes. Therefore, surgeons in LMICs need a device which can be manufactured locally, with materials costing less than 60 USD, that provides an accurate way to monitor the exact levels of maternal blood loss in real-time during C-section. Additionally, the device must be easy to use, and be sterilizable.
Our solution is the Hemosave device. Doctors use the Hemosave device by aspirating blood and amniotic fluid lost during surgery into the device. The blood is analyzed constantly using gravimetric and spectrophotometric techniques, and the exact volume of blood lost is displayed, in milliliters, for healthcare professionals to see.
Duke University Student Design Team:
Desmond Boateng, James Bradley, Mohammed Farah, and Haasini Nandyala
Automated Catheter Lamination and Heat Shrink Platform
University of Texas at Austin Student Design Team:
Daniel Smith, Blanca Cuesta, and Iman Salafian
Instructor: Prof. Christopher G. Rylander
Clinical Advisor: Dr. Alan Groves
A New Pallet and Restraint System for Pediatric Nuclear Medicine

Nuclear imaging can be used to diagnose a variety of diseases, including, but not limited to, hydronephrosis, osteoarthritis, bone cancer, and acute tubular necrosis. Pediatric patients subjected to these scans require that the nuclear imaging device be modulated to accommodate the smaller size of the patient. Various pediatric modulatory devices for nuclear imaging machines are available, however they are either single-use, do not provide a suitable restraint method, have a very small patient height/size range, or are designed for and sold in conjunction with a specific nuclear imaging machine and not cross-compatible to be used with another machine. A new pediatric pallet with effective restraints, that is compatible with a range of nuclear imaging devices, reusable, and can be used on children of various heights could help fill the large gap in the market of such devices. Our value proposition is that we provide a proper sized pediatric pallet with a built-in restraint system to ease the process of nuclear imaging for both the technologists and patients.
University of Alabama at Birmingham Student Design Team:
Andrew Budisalich, Brianna Emperley, Christopher Morgan, Evan Henry, and Eve Scott
InVenimus: Ultrasound-Securing Armband for Intravenous Access in Pediatric ER

Peripheral intravenous (PIV) lines establish minimally-invasive vascular access for the delivery of fluids and medication in emergency room patients. Ultrasound guidance allows for venous visualization during PIV placement, however IV operators face challenges while obtaining vascular access in pediatric patients aged 12-36 months. This is due to their higher subcutaneous fat and smaller vein diameters when compared to healthy adults.
InVenimus has developed an armband that secures an ultrasound probe to a pediatric patient’s arm. This device allows the IV operator to use both hands to insert the needle, increasing the success rate of PIV placement on the first attempt. By reducing the need for a second attempt, InVenimus aims to decrease the time required for patient stabilization in emergency rooms.
Johns Hopkins University Student Design Team:
Saardhak Bhrugubanda, Ankur Govil, Nehali Gupta, Ashish Nalla, Thienviet Ngomai, Govardhan Poondi, Valerie Tu, Amy Zhang, Dr. Constanza Miranda, Kelsey Detels, and Dr. Badaki-Makun
Glow and Sew: A Fluorescent Suture and Surgical Planner for Image Guided Surgery

Anastomosis involves the sewing of two tissues during the reconstructive phase of a surgical procedure. The technique is performed over a million times a year in the United States, and is most common in cardiovascular, gastrointestinal, and visceral surgeries. Anastomosis is considered one of the most critical steps of a surgery, because a single misplaced suture may result in postoperative complications which significantly undermine clinical outcomes, increase patient mortality up to ten times, diminish a patient’s quality of life, and may require corrective surgery. Anastomotic leak is the most dreaded and morbid complication occurring in up to 20% of patients. There exists a clinical need for a tool and technique to improve the consistency of anastomosis and minimize the rate of postoperative surgical complication.
We developed Glow and Sew, a novel near infrared fluorescent (NIRF) suture and AI-based surgical planner to improve anastomosis outcomes for image guided and robotic surgeries. NIR cameras and dyes are already used clinically to illuminate the bile duct during cholecystectomy so that it remains visible when covered by tissue. By embedding these same fluorescent dyes into our product, the surgeon has constant visualization of the suture line during anastomosis, even when the suture is occluded by blood and tissue. The AI-based planner expands the utility of the NIRF sutures by using the suture locations as landmarks to create intraoperative surgical guides. The software identifies the start and end of the suture line, the current suture location, and overlays the ideal “next suture” position which acts as a patient specific suturing template to standardize anastomosis outcomes independent of surgeon training or skill.
Johns Hopkins University Student Design Team:
Justin Opfermann (Left), Yaning Wang (Middle), Jiawei Ge (Right)
Johns Hopkins University Faculty Mentors: Dr. Axel Krieger, Dr. Jin U. Kang, Dr. Minjae Do
Tailored Brachytherapy Solutions: A Novel Cervical Cancer Treatment Device

Tailored Brachytherapy Solutions (TBS) aims to address the challenge of customizing brachytherapy devices for cervical cancer patients. TBS proposes a system of interchangeable applicator tips that can be inserted into a standard obturator base, gliding sleeves and a positioning template. The custom applicator tips are designed to accommodate a wider range of patient anatomy. A custom hexagonal template allows for increased range of motion of needle placement and a smoother glide into position. TBS is optimizing material selection for sterilization and specific properties desired by clinicians, saving time and money by enabling in-house 3D printing and reusability. Overall, Tailored Brachytherapy Solutions aims to improve the precision, flexibility, and biocompatibility of brachytherapy devices, benefiting patients, healthcare providers and medical institutions.
Milwaukee School of Engineering Student Design Team:
Alexandria Such, Zoe Rush, Emma Braun, Katherine Goberman, and Jordyn Sievert
Photo (Left to Right): Emma Braun, Katherine Goberman, Jordyn Sievert, Alexandria Such, Zoe Rush
CannuFlow: Optimizing Distal Blood Flow in the pVA-ECMO Arterial Cannula

Peripheral veno-arterial extracorporeal membrane oxygenation (pVA-ECMO) is a medical procedure to temporarily support a patient’s heart and lungs by pumping and oxygenating the blood. Limb ischemia is a common complication in this patient population, occurring when the blood flow is cut off distally at the site of femoral arterial cannulation. The CannuFlow is a device that tackles the concern of limb ischemia by providing distal and proximal flow at a single insertion site.
University of Iowa Student Design Team:
Sushma Santhana, Nyvaeh Bowen, Ethan Pierce, and Anne Cunningham
Melanin Stratifying Device: Elastic Scattering Spectroscopy to Diagnose RLS

Restless Leg Syndrome (RLS) is a neurological sensory-motor disorder characterized by creeping sensations and restlessness deep inside the lower legs. Although 7 to 10 percent of the United States population is affected by this condition, a limited number of objective criteria are used to make clinical diagnoses for RLS and no cure exists. A collaborator on the project recently found that RLS symptoms were triggered when administered alpha-melanocyte stimulating hormone (α-MSH), which is stimulated by melanin. Our probe uses elastic scattering spectroscopy (ESS) to extract optical properties of the skin from the UV-to-visible wavelength spectrum, which are sensitive to the absorption and scattering effects due to melanin seen in diverse skin tones. By stratifying melanin with ESS measurements, we can develop a novel method of identifying biomarkers for RLS based on melanin absorbance and work towards enhancing RLS diagnosis. This device holds promise for advancing RLS patient care outcomes and even into the realm of dermatology.
Boston University Student Design Team:
Sarah Wolf, Arjavi Vyas, Maks Levin, Tyler Sanabria, and Ethan Bosworth
Arterial Line Training Device

Team PATS from Duke University's Biomedical Engineering department, comprising if three sophomores have developed Pulse Mate, a system aimed at improving arterial line insertion training. With an emphasis on addressing the lack of effective training methods, Pulse Mate offers a cost-effective solution priced at $190 to make, and capable of enduring up to 50 daily uses. This innovative device simulates the feel and pulsation of a human arm, featuring multiple skin tones for a realistic training experience. Unlike existing arterial line placement trainers, which often require manual pulse simulation and exhibit costly maintenance, Pulse Mate stands out with its user-friendly touchscreen interface and electronic pulse simulation capability. Notably, the device allows for catheter threading and blood drawing simulation, facilitating comprehensive training. Tested at Duke Hospital's Simulation Center and validated by attending physicians and residents, Pulse Mate garnered positive feedback, scoring high on realism and ease of use. Feedback also provided valuable insights for further enhancements, emphasizing the device's utility as a training tool for medical professionals nationwide.
Duke University Student Design Team:
Christopher Wyrtzen, Nicholas Trigger, and Ryan Blue
Influx: A Novel Approach to Patient Specific Opioid Addiction Recovery

InFlux is a pod-like wearable device that delivers continuous doses of Naltrexone into the bloodstream of those with opioid abuse disorder and alcohol use disorder to alleviate substance withdrawal symptoms. This provides users with a more streamlined and functional method to administer anti-withdrawal medication easily. In addition to the more streamlined nature of our method of delivery, InFlux also provides patients with a steady dosage of naltrexone over time, helping to reduce peaks and dips in the concentration of the drug in the patient’s system, which can help reduce risk of relapse and the pain of withdrawal symptoms. InFlux facilitates communication between patient and doctor as well as patient and community to give additional support during the treatment process. Many patients are also hesitant to use the long-lasting injectable form of naltrexone, as it will block pain medications in the case of emergency, forcing doctors to administer stronger and more dangerous pain medications. InFlux addresses these logistical concerns of naltrexone by providing a more convenient and widely applicable solution. Combining its bioinformatic design with its remotely accessible user interface, InFlux guarantees a smooth recovery experience for patients regardless of location and access to immediate care. InFlux allows physicians to carefully monitor treatment plans, adjust dosages, and exchange messages with patients in a time-efficient manner in response to their patients’ condition. The device also enables physicians to treat patients in remote and underserved areas, addressing the spatial inequality abundant in the US, and ensuring equitable healthcare delivery. It is remotely accessible via a secure app, matching the progressively digitizing landscape of healthcare, and can reach afflicted patients more quickly, delivering urgent relief in seconds to someone experiencing withdrawal.
Cornell University Student Design Team:
Ashmitha Sivakumar, Tej Ramachandrula, Shanie Zeltzer, Shruti Nagpal, Sruti Gudapati, David Musheyev, Avinaash Kantamneni, Claire Walter, Minjae Eum, Paris Chakravarty, Aaryan Pugazendhi, and Maya Nitta